14 YR MALE PRESENTED WITH HISTORY OF PASSING BLOOD IN STOOLS AND URINE FOR 2 DAYS
Anigani Kavya
Roll number- 06
4th year MBBS
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
CASE DISCUSSION
A 14year old male patient resident of Suryapet has come to the OPD with
1.History of passing blood in stools and urine for 2days (2 episodes)
2.Lethargy from 1week
History of presenting illness:
Patient was born out of consanguineous marriage, 4th child to his parents, 3 elder siblings, 2 sisters and 1 brother.
Patient was apparently asymptomatic 6 years back later he developed sudden generalized weakness and was taken to hospital in an altered mental state.
Patient was evaluated and found to have type 1 diabetes mellitus. He was advised insulin since then.
3years back patient again developed similar complaints for which insulin dose was increased.
Hyperpigmentation of skin, both hands and feet,around the mouth and neck since 6months.
1month back he developed involuntary movements in hands and feet, found to have hypoglycemia.
Patient was also found to have low HB, WBC,RBC, PLT
Patient was managed conservatively and discharged after which he developed current symptoms within 2days
17.8.2021
He was admitted in Osmania, 2 blood transfusions were done
Before transfusion HB- 2.7
After transfusion HB- 7.8
Vitamin B12 levels- 150
PAST HISTORY:
Know case of Type 1 DM since 6years
No H/O HTN, Asthma, TB
PERSONAL HISTORY:
PERSONAL HISTORY:
Diet: Mixed
Appetite: Reduced from past 2months
Bowl and bladder movements- Regular
Sleep: Inadequate
Appetite: Reduced from past 2months
Bowl and bladder movements- Regular
Sleep: Inadequate
No addictions
FAMILY HISTORY : NOT SIGNIFICANT
FAMILY HISTORY : NOT SIGNIFICANT
GENERAL EXAMINATION :
Patient is conscious, coherent and cooperative, well oriented to time,place and person.
Patient is conscious, coherent and cooperative, well oriented to time,place and person.
Vitals:
Blood pressure:100/60mmHg
Pulse rate-70 BPM
GRBS- 217
Afebrile
Height -119 cms
Weight -22 kgs (Height weight less than 3 rd percentile)
Pallor- present
Icterus- present
Weight -22 kgs (Height weight less than 3 rd percentile)
Pallor- present
Icterus- present
Cyanosis- absent
Clubbing- absent
Lymphadenopathy- absent
Hyperpigmented knuckles +
Single palmar crease
Hyperpigmented patches over the palate seen
Hyperpigmented knuckles +
Single palmar crease
Hyperpigmented patches over the palate seen
Suggestive features of Down's syndrome:
-Short stature
-Gap between 1st and 2nd toe
-Palmar crease
-Epicanthic eye fold
INVESTIGATIONS:
1.9.21
Hemogram:Prothrombin Time:
Reticulocyte count:
Blood parasites (MP):
Urinary sodium:Urinary Potassium:
Urinary chloride:
Urine protein/creatinine ratio:
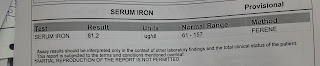
Serum iron:
Stool for occult blood:Combs test:
Albumin-2.8
Urea: 151
Creatinine- 3.5
ECGUSG
Impression:
Mild ascites
Thin internal echos noted in Urinary bladder
Cross consultation reports:
Dermatology
Ophthalmology
ENT
Dental
Surgery:
Provisional diagnosis:
Down's syndrome
Autoimmune polyglandular syndrome- II
(type 1 diabetes,addisons)
Vitamin B12 anemia with hemolysis.
?Hemolytic uremic syndrome.
Fissure in ANO
Treatment:
1.9.21 (Day 1)
1.INJ Vit B12 1000mcg IV OD
2.Insulin drip according to sliding scale
3. Tab MVT PO OD
4. I/O charting
2.9.21 (Day 2)
1.INJ VIT B12 1000mcg IV OD
2.IVF- NS @75ml/hr
3..INJ HAI S/C TID
4.INJ NPH S/C BD
5.GRBS profile
6.BP/PR/TEMP/RR MONITORING 12th Hourly
7.I/O charting
3.9.21 (Day 3)
1.INJ VIT B12 1000mcg IV OD
2.IVF- NS @75ml/hr
3..INJ HAI S/C TID
4.INJ NPH S/C BD
5.GRBS profile
6.BP/PR/TEMP/RR MONITORING 12th Hourly
7.I/O charting
4.9.21 (Day 4)
1.INJ VIT B12 1000mcg IV OD
2.IVF- NS @75ml/hr
3..INJ HAI S/C TID
4.INJ NPH S/C BD
5.ZyTEE gel for L/A on oral mucosa before food
6.Ciproflox-D ear drops
7.GRBS monitoring
Questions
1. What is the cause of blood in stool and urine in this patient?
2. What causes Autoimmune polyglandular syndrome type 2? Is it inherited?



































buy methyl testosterone online
ReplyDeleteAnavar for sale
Testosterone cypionate for sale
depo testosterone for sale
buy clenbuterol
Arimidex for sale
buy botox online
buy testosterone online