60 year old male with fever and SOB and Right LL swelling since 3days
Anigani Kavya
Roll number- 06
4th year MBBS
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
A 60 year old male patient from dhamera village came to casuality with chief complaints:
-Fever since 3 days
-SOB grade 2----> 4 since 2 days
-Right LL swelling and redness since 1 days
History of presenting illness:
Patient was apparently asymptomatic 3 days back and then he developed fever which was low grade, intermittent, relieved on taking medication and not associated with chills and rigor.
He has SOB (grade 2 which later progressed to grade 4) No orthopnea or PND or pedal edema or chest pain or palpitations.
He applied ointment for leg pain over right foot 3days back and later he developed redness and swelling over right foot (no history of trauma or injury) with these complaints they went to outside hospital and on presentation to the outside hospital vitals spO2-74% on RA with, BP 70/40 and Decreased urine output.All necessary Investigations were done and he was treated with IV Antibiotics, IV antacids, IV nebulization, IV iontropes, IV multivitamins, He was put on CPAP, and his conditions was explained and was advised for hemodialysis. But patient attendees was not willing for further investigation and wanted to refer to our hospital.
General Examination:
Patient is conscious, coherent and cooperative. Well oriented to time, place and person
No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy, edema
Vitals:
Temp - 100 F
PR- 104 bpm
BP- 100/70mmHg
RR- 28 cpm
SpO2- 97% at RA
Systemic Examination:
CVS: S1 S2 heard
RS: Decreased BAE
B/l crepts present in IAA and ISA
P/A: soft and non tender
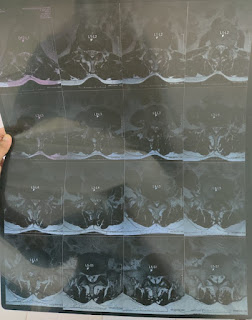
Clinical images:
































Comments
Post a Comment